Corneal abrasion + bacteria/infective element corneal abrasion (infective keratitis)
Sight threatening infection
- Inflammation of the cornea
- Bacterial and viral are the most common - rarely fungal or protozoan
| Pathogens | Clinical features | Management | |
|---|---|---|---|
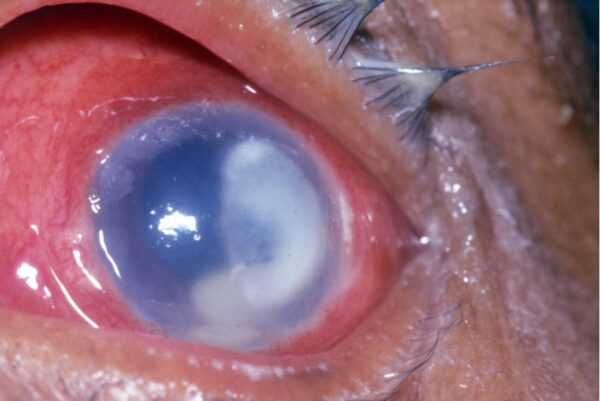
| Bacterial | - Pseudomonas spp. - Staphylococcus spp. - Streptococcus spp. | - Mucopurulent discharge - Yellow-white infiltrate with clearly defined margins - Hypopyon + | - Topical antibiotics (chloramphenicol), and steroids - +/- oral antibiotics |
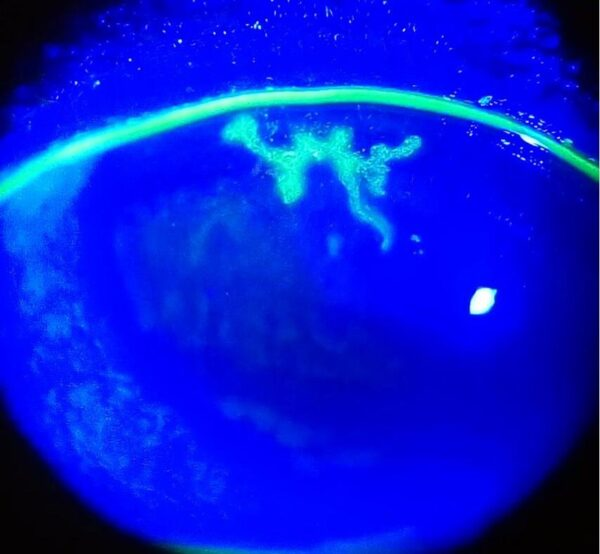
| Viral | - Herpes Simplex Virus - Varicella zoster virus | - Clear discharge / epiphora - Epithelial defect with linear branching and terminal bulbs (dendritic ulcer) - Reduced corneal sensation - Hypopyon – | - Topical antivirals (acyclovir) and cycloplegics |
| Fungal | - Aspergillus spp. - Fusarium spp. - Candida spp. | - Mucopurulent discharge (less than bacterial) - Grey-white infiltrate with fluffy margins and satellite lesions - Hypopyon + | - Topical antifungals - +/ topical antibiotics - +/- systemic antifungals |
| Protozoan | - Acanthamoeba spp. | - Clear discharge / epiphora - Ring-shaped infiltrate - Reduced corneal sensation - Hypopyon +/- | - Topical PHMB and chlorhexidine |
Bacterial
- Staph, Strep, Pseudomonas spps in patients with a distrupted corneal epithelium
- Neisseria honorrhoeae, Neisseria meningitides, Corynebacterium diphtheria can penetrate an intact epithelium
Risk factors:
- Contact lens wear - most common factor esp in prolonged used and poor hygiene
- Corneal trauma
- Ocular surface disease - dry eye, lid malposition, Blepharitis
- Immunosuppression
Features - usually causes unilateral symptoms:
- Ocular pain
- Red eye
- Reduced visual acuity
- Photophobia
- Purulent discharge
Investigations
-
Contact lens wearing history, type of lens, duration per day, slept showered or swam with lenses in
-
Corneal scrapes and conjunctival swabs
-
Contact lenses cases solutions should also be sent for MC&S
-
Sign & symptoms
- Lids and lashes - eyelid oedema in moderate to severe cases
- Conjunctiva - pattern of injection may be circumlimbal or diffuse
- Cornea - yellow opacity with clear margins Epithelial defect will stain green upon fluroescein drops under blue light
Management
- Stop contact lens use immediately
- Topical antibiotics - initially broad spectrum (fluoroquinolone or cefuroxime and Gentamicin) until culture returns
- Oral antibiotics in severe cases
Complications:
- Spread of infection: the infection may spread beyond the cornea into the sclera or within the deeper tissues of the eye, leading to endophthalmitis.
- Corneal perforation in severe cases
- Residual dense corneal scarring
- Irregular astigmatism
- Formation of cataract: secondary lens opacification is common following severe inflammation
The overall visual outcome is very variable and dependent on a number of factors which include the size and depth of the infection, time to diagnosis and initiation of treatment, and compliance with therapy.
Viral keratitis
- Primary infection with HSV usually acquired in childhood and commonly mild or sub-clinical (symptoms of blepharoconjunctivitis and URTI)
- Latency in trigeminal ganglion - upon reactivation travels back to periphery such as corneal epithelium - epithelial keratitis
Risk factors
- Direct contact with infected secretions or lesions
- Reactivation via trauma to trigeminal nerve, stress, Immunosuppression, previous reactivation
Each attack is associated with a greater is of recurrence
Clinical features
- Same as other forms of keratitis
- Epiphora (watering of eyes) as opposed to purulent discharged seen in bacterial
- Cornea - dendritic ulcer (pathognomonic sign) with linear branching morphology and terminal bulbs.
- Bed of the ulcer will stain green with fluroscein while the ulder magin with stain with rose Bengal
- Reduced corneal sensation
Investigations:
- HSV keratitis can be diagnosed clinically with the identification of dendritic ulder
- Swabs sent for PCR
Management
- Stop contact lens use
- Topical Antivirals (aciclovir 3% ointment 5 time a day for up to 2 weeks)
- Epithelial debridement - to reduce viral load and promote healing
- May need long term oral anti-viral prophylaxis
Steroids are contraindicated in active epithelial disease
Only used in close supervision by ophthalmologists to suppress the immune response i cases with corneal stromal involvement
Most resolve even without treatment
Herpes zoster ophthalmicus (HZO)
- Reactivation of the VZV affecting the ophthalmic branch of trigeminal nerve (V1)
- On examination under fluorescein, small dots (punctate keratitis) or pseudo-dendrites (lacking terminal bulbs, in contrast to HSV keratitis) may be visible on the cornea.
- HZO can affect any part of the eye or orbit
Fungal
- Uncommon but aggressive
- Major cause of visual loss
- Commonly associated with fusarium and aspergillus species (filamentary fungi)
- Candida species in the immunocompromised
Risk factors
- Same as bacterial
Clinical features
- Lids and lashes: redness and periocular oedema
- Conjunctiva: diffuse injection
- Cornea: grey-white stromal infiltrate with fluffy margins. Satellite lesions may be seen. Rapid progression may occur with necrosis and corneal thinning
- Anterior chamber: inflammation, evidenced by the presence of cells, or hypopyon in severe cases
Investigations
- Corneal scraping - Gram and Giemsa staining and culture
- PCR
Management
- Contact lens stop immediately
- Topical anti-fungals hourly iitially and them tapered according to response
- Systemic anti-fungals in severe and immunocompromised cases
- Oral analgesia and topical cycloplegia
- Topical steroids should be avoided in the acute phase but may then be considered during stages of healing
Complications
Visual prognosis is generally poor due to high rate of complications. Recurrence is common after tapering treatment off
Other complications include:
- Severe inflammatory response leading to Scleritis
- Corneal perforation
Acanthamoeba keratitis
Rare form of microbial keratitis associated with poor visual outcomes
- Free living protozoa isolated from soil, pond, tap and chlorinated water.
- In developed countries vast majority of patients are contact wearers
Clinical features
- Pain is severe disproportionate to relatively mild clinical findings
- Lids and lashes: mild swelling and erythema
- Conjunctiva: diffuse injection
- Cornea: classically a ring-shaped infiltrate with radial perineural infiltrates
- Pseudodendrites (similar to HZO)
- Reduced corneal sensation
Investigations
- Corneal scrape - PCR, culture and histology
- Contact lenses, cases and solutions for MC&S Corneal biopsy may be considered in culture negative cases
Management
- Contact lens stop bad >:(
- Topical antiamoebic agents - topical polyhexamethylene biguanide 0.02% or chlorhexidine 0.02%
- Oral NSAIDs for pain management
- Topical steroids
- Penetrating keratoplasy considered in cases with severe corneal scarring or extensive necrosis
Complications
- Extension of disease to involve the sclera
- Recurrent infection
- Corneal perforation
Overall, the prognosis is poor compared to other forms of microbial keratitis. Prevention is therefore vital. Contact lens wearers should be educated on avoidable risk factors and be encouraged to seek medical attention early when symptoms develop.