Bleeding into the space between the arachnoid membrane and the pia mater - subarachnoid
Causes/Factors
- Aneurysms: Berry Aneurysm rupture (80%) - common locations: junctions of posterior communicating with the internal carotid artery or anterior communicating with anterior cerebral artery
- Trauma: Head injury or trauma can lead to bleeding.
- Arteriovenous Malformations (AVMs): Abnormal connections between arteries and veins in the brain.
- Blood-Thinning Medications: Medications like Anticoagulants can increase the risk of bleeding.
- Family History: A family history of aneurysms or SAH 3-5x risk
- Other conditions: That increase risk of aneurysms eg Ehlers-Danlos syndrome, Polycystic Kidney Disease
Symptoms
- Severe Headache: “Thunderclap” headache
- Neck Pain and Stiffness: Due to irritation of the meninges
- Nausea and Vomiting: Often accompanied by the headache.
- Altered Consciousness: Confusion, loss of consciousness, or coma.
- Seizures: In some cases.
- Sensitivity to Light (Photophobia) and Sound (Phonophobia): Due to increased intracranial pressure.
Signs
- Positive Kernig’s and Brudzinski’s Signs: Takes 6h to develop - Pain on passive extension on knee and passive flexion of neck
Diagnostic Tests
- Urgent CT - detects over 95% of SAH within 24h
- LP if CT is -ve and history is very suggestive. Must be done 12+ hours after headache onset to allow for breakdown of RBCs
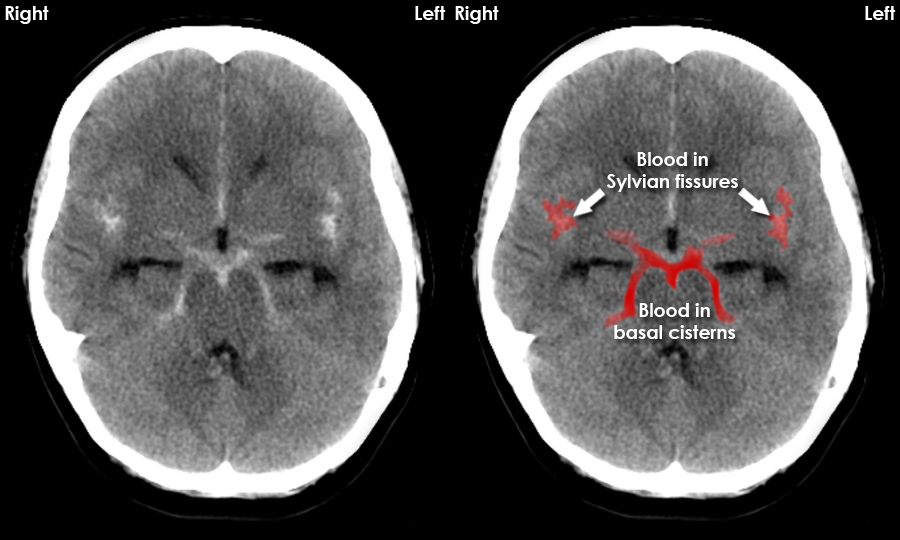 Starfish appearance on CT
Starfish appearance on CT
Management
Refer all confirmed SAH to neurosurgery
- Re-examine to determine if condition worsening - possible repeat CT
- Blood pressure control - <160mmHg
- Nimodipine 60mg/4h for 3wks (Ca antagonist to prevent vasospasm)
Surgery: endovascular coiling vs surgical clipping depends on location of Aneurysm, but coiling is preferred
Complications/red Flags
- Rebleeding is the commonest cause of death and occurs in 20%
- Vasospasm leading to cerebral ischaemia may cause permanent CNS deficit and commonest cause of morbidity
- Hydrocephalus due to blockage of arachnoid granulations requires a shunt or drain