Most common form of breast cancer in the UK - around 1 in 8 lifetime risk for women (1% of UK cases are male)
Types
Non-invasive ductal carcinoma in situ (DCIS)
- Pre-malignant cancer of epithelial cells of breast ducts
- Localised to a single area
- Often picked up by mammogram screening
- Potential to spread locally over years
- 30% become invasive
- Good prognosis if excised and adjuvant treatment
Lobular carcinoma in situ (LCIS)
- Pre-malignant typically in pre-menopausal women
- Rarer and tends to be multifocal
- Increased risk of invasive breast cancer in the future (~30%)
- Often managed conservatively with monitoring (6 monthly exam and yearly mammogram)
Invasive ductal carcinoma - NST
- Most common invasive carcinoma (80%)
- NST - means no specific type and its not specifically classified (eg medullary or mucinous)
- Originate in cells from the breast ducts
- Can be seen on mammograms
Invasive lobular carcinomas
- Around 15% of invasive breast cancers
- Originate in cells from the breast lobules
- Not always visible on mammograms
Inflammatory breast cancer
- 1-3% of carcinomas
- Presents similarly to a Breast abscess or mastitis
- Swollen, warm, tender breast with pitting skin (peau d’orange)
- Does not respond to antibiotics
- Worse prognosis than other breast cancers
Paget’s Disease of the Nipple
- Looks like eczema of the nipple/areolar
- Erythematous, scaly rash
- Indicates breast cancer involving the nipple
- May represent DCIS or invasive breast cancer
- Requires biopsy, staging and treatment, as with any other invasive breast cancer
Rarer Types of Breast Cancer
- Medullary breast cancer
- Mucinous breast cancer
- Tubular breast cancer
- Multiple others
Causes/Factors
- Family history - first degree (BRCA1/2 gene)
- BRCA1 gene on chromosome 17
- Around 70% will develop breast cancer by 80
- Around 50% will develop Ovarian Cancer
- Also increased risk of bowel and prostate
- BRCA2 gene on chromosome 13
- Around 60% will develop breast cancer by aged 80
- Around 20% will develop Ovarian Cancer
- BRCA1 gene on chromosome 17
- Increased oestrogen exposure (earlier onset of periods and later menopause; nulliparity; 1st Pregnancy 30>yrs old)
- More dense breast tissue - more glandular tissue
- Obesity
- Smoking
Presentation
- Lumps that are hard, irregular, painless or fixed in place
- Lumps may be tethered to the skin or the chest wall
- Nipple retraction
- Skin dimpling or oedema (peau d’orange)
- Lymphadenopathy, particularly in the axilla
Referral Criteria
Two week wait referral for:
- Unexplained breast lump in patients aged 30 or above
- Unilateral nipple changes in patients aged over 50 or above
- Unexplained lump in the axilla in patients aged 30 or above
- Skin changes suggestive of breast cancer
Investigations
Triple assessment
- Clinical assessment (history and examination)
- Imaging (ultrasound or mammography)
- Biopsy (fine needle aspiration or core biopsy)
-
Ultrasound scans are typically used to assess Lumps in younger women - distinguish solid Lumps from cystic fluid
-
Mammograms are generally more effective in older women - can find calcifications
-
MRI for screening women in higher risk groups or to further assess the size and features of a tumour
-
Sentinel lymph node biopsy may be used during breast cancer surgery where the initial ultrasound does not show any abnormal nodes.
- Contrast in injected into the tumour area and travels through the lymphatics to the first lymph node - sentinel.
-
Cancer histology - may have receptors:
- Oestrogen receptors (ER)
- Progesterone receptors (PR)
- Human epidermal growth factor (HER2) Triple-negative breast cancer is where the breast cancer cells do not express any of these three receptors. This carries a worse prognosis, as it limits the treatment options for targeting the cancer.
Breast cancer screening
The NHS breast cancer screening program offers a mammogram every 3 years to women aged 50 – 70 years.
Screening aims to detect breast cancer early, which improves outcomes. Roughly 1 in 100 women are diagnosed with breast cancer after going for a mammogram.
High risk patients
There are different recommendations for screening patients with a higher risk.
- Genetic Counselling
- Annual mammogram
- Chemoprevention
- Tamoxifen (ER modulator) if premenopausal
- Anastrozole (prevents conversion of androgens to oestrogen) if post (except with severe osteoporosis)
Management
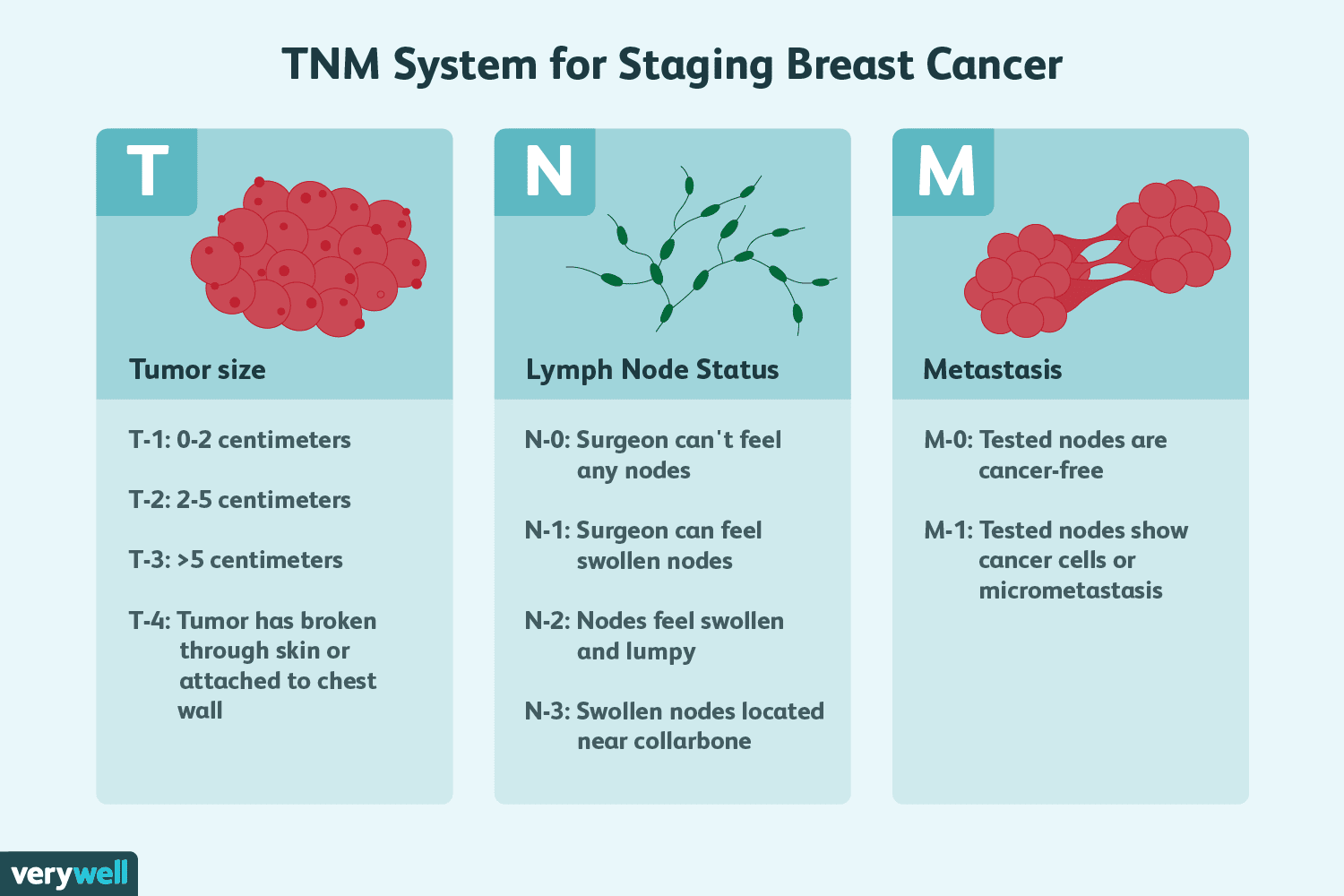
TNM staging:
All patients are discussed with the multidisciplinary team (MDT) for treatment planning
Surgery
- Tumour removal
- Axillary clearance
- Reconstructive - immediate or delayed. Can be partial or reduce and reshape both breasts to match
Radiotherapy
Chemotherapy
- Neoadjuvant therapy – intended to shrink the tumour before surgery
- Adjuvant chemotherapy – given after surgery to reduce recurrence
- Treatment of metastatic or recurrent breast cancer
Drug treatment
- Tamoxifen for premenopausal
- Aromatase inhibitors for post
ER positive
- Fulvestrant (selective ER down regulator )
- GnRH (Gonadotropin releasing hormone)
HER2 positive
- Herceptin (trastuzumab) - monoclonal antibody targets HER2 receptor. Can also affect heart function so initial heart monitoring is required
- Perjeta (pertuzumab) for HER2 receptor can be used in combination with herceptin
- Nerlynx (neratinib) - tryosine kinase inhibitor reducing the growth of breast cancers
Complications/red Flags
Metastasis
- Lungs - Liver
- Bones
- Brain
Chronic lymphoedema = impaired drainage in that area
Cannulas and bloods
Avoid taking blood or putting a cannula in the arm on the side of previous breast cancer surgery. Higher risk of complications and infections due to the impaired lymphatic drainage on that side