Introduction
- Wash hands (and don PPE if needed)
- Introduce yourself (name and role)
- Confirm patient’s name and DOB
- Explain what the examination involves
- Gain consent to continue
- Ask if patient in any pain before continuing
General Inspection
Clinical Signs
- Cyanosis
- Shortness of breath (congestive Heart Failure, Pericarditis pneumonia, pulmonary embolism)
- Pallor - not very sensitive - paleness → anaemia (haemorrhage, chronic disease) or poor perfusion (congestive Heart Failure)
- Malar flush - plum red discolouration of the cheeks associated with Mitral stenosis
- Oedema - lots of causes, usually in limbs (pedal) or abdomen (Ascites). Usually in context of CVS exam congestive Heart Failure
Objects and Equipment
- Oxygen
- Bedside equipment - ECG, ECHO machine
- GTN spray/medication
Hands
Inspection
- Colour - pallor → poor peripheral perfusion and cyanosis
- Tar staining - smoking, risk factor for CVD
- Xanthomata - yellow cholesterol-rich deposits
- Arachnodactyly - fingers and toes abnormally long and slender, feature of Marfan’s syndrome mitral/aortic valve prolapse & aortic dissection
- Splinter haemorrhages - local trauma, infective endocarditis, sepsis, vasculitis
- Janeway lesions and Osler’s nodes - infective Endocarditis
- Pale palmar creases - anaemia
Finger Clubbing
- Schamroth’s window test - congenital cyanotic heart disease, infective Endocarditis, and atrial myxoma
Palpation
Temperature
Place dorsal aspect of your hand onto patients to assess temperature
Capillary Refill time
- Apply 5 seconds of pressure onto finger and release
- Should return in <2 seconds
- If >2 seconds suggests poor peripheral perfusion (hypovolaemia, congestive heart failure) and need to assess central cap refill
Radial Pulse - Rhythm and Rate
- Palpate for 30 seconds - 60 if irregular
- Irregular rhythm is most commonly caused by Atrial Fibrillation
Radio-radial Delay
Palpate both radial pulse together. If out of sync +ve test. Causes include:
- Subclavian artery stenosis (e.g. compression by a cervical rib)
- Aortic dissection
- Aortic coarctation
Collapsing Pulse
A collapsing pulse is a forceful pulse that rapidly increases and subsequently collapses. Ask patient if in any pain in shoulder as going to have to move it rapidly Causes of a collapsing pulse:
- Aortic regurgitation
- Thyrotoxicosis
- Anaemia
- Pregnancy
- AV fistula
Blood Pressure
Tell the examiner that you would like to take one In a cardiovascular examination OSCE station, you are unlikely to have to carry out a thorough blood pressure assessment due to time restraints, however, you should demonstrate that you have an awareness of what this would involve.
Face
- General colour
- Malar flush - Mitral stenosis
Eyes
- Xanthelasma - yellow bits on eyelids - hypercholesterolemia
- Corneal arcus - blue-grey ring around iris - hypercholesterolemia - Pallor of conjunctivae – pull down eyelid, anaemia
Lips and tongue
- Blue lips - peripheral cyanosis
- Blue under the tongue - central cyanosis - hypoxaemia - possible shunt?
- General dental hygiene - Endocarditis
- Angular stomatitis - anaemia
- High-arched palate - Marfan’s syndrome
Neck
Carotid Pulse
Auscultate
Prior to palpating the carotid artery need to rule out the presence of a bruit - which indicates carotid stenosis
-
Place bell of stethoscope over carotid pulse
-
Ask patient to take a deep breath in and hold
-
Sound of a carotid bruit
-
The presence of a ‘carotid bruit’ may, in fact, be a radiating cardiac murmur
Palpate
If no bruits were identified, proceed to carotid pulse palpation: 1. Ensure the patient is positioned safely on the bed, as there is a risk of inducing reflex bradycardia when palpating the carotid artery (potentially causing a syncopal episode). 2. Place fingers on carotid 3. Assess the character (e.g. slow-rising, thready) and volume of the pulse.
Jugular Vein
Jugular Venous Pressure
Indirect measure of central venous pressure (IJV connects to right atrium without any valves). Causes include Right Heart Failure, Tricuspid regurgitation and constrictive Pericarditis
- Position the patient in a semi-recumbent position (at 45°).
- Ask the patient to turn their head slightly to the left
- Inspect for evidence of IJV running between the medial end of the clavicle and the ear lobe, under the medial aspect of the sternocleidomastoid
- Measure the JVP by assessing the vertical distance between the sternal angle and the top of the pulsation point of the IJV (in healthy individuals, this should be no greater than 3 cm).
Hepatojugular Reflux Test (not Performed in an OSCE)
The hepatojugular reflux test involves the application of pressure to the liver whilst observing for a sustained rise in JVP.
- In healthy individuals, this rise should last no longer than 1-2 cardiac cycles (it should then fall).
- If the rise in JVP is sustained and equal to or greater than 4cm this is deemed a positive result.
A positive hepatojugular reflux result suggests the right ventricle is unable to accommodate an increased venous return, but it is not diagnostic of any specific condition. Constrictive pericarditis, right and left ventricular failure and restrictive cardiomyopathy can cause a positive result
Chest
Inspect
- Scars suggestive of previous thoracic surgery
- Pectus excavatum: a caved-in or sunken appearance of the chest.
- Pectus carinatum: protrusion of the sternum and ribs.
- Visible pulsations: a forceful apex beat may be visible secondary to underlying ventricular hypertrophy.
Palpation
Apex Beat
- Typically located in 5th intercostal space in midclavicular line
- Displacement of apex beat from its usual location can occur due to anything that shifts mediastinum
Heaves
A parasternal heave is a precordial impulse that can be palpated.
- Place the heel of your hand parallel to the left sternal edge (fingers vertical) to palpate for heaves.
- If heaves are present you should feel the heel of your hand being lifted with each systole.
- Parasternal heaves are typically associated with left or right ventricular hypertrophy.
Thrill
A thrill is a palpable vibration caused by turbulent blood flow through a heart valve (a thrill is a palpable murmur). You should assess for a thrill across each of the heart valves in turn
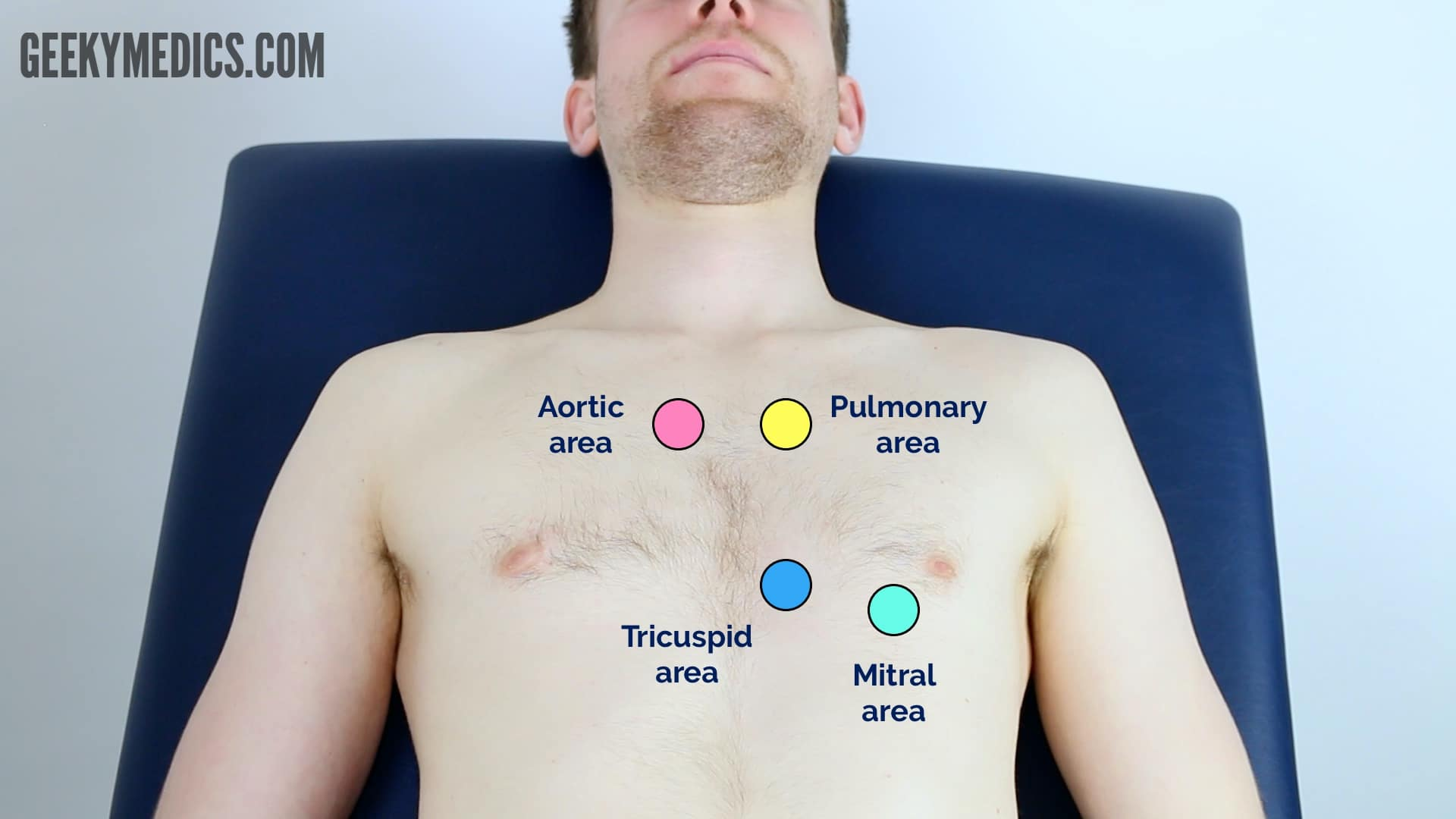
Auscultation
- Palpate the carotid pulse to determine the first heart sound.
- Auscultate ‘upwards’ through the valve areas using the diaphragm of the stethoscope whilst continuing to palpate the carotid pulse:
- Aortic valve: 2nd intercostal space at the right sternal edge.
- Pulmonary valve: 2nd intercostal space at the left sternal edge.
- Tricuspid valve: 4th or 5th intercostal space at the lower left sternal edge.
- Mitral valve: 5th intercostal space in the midclavicular line.
Accentuation Manoeuvres
-
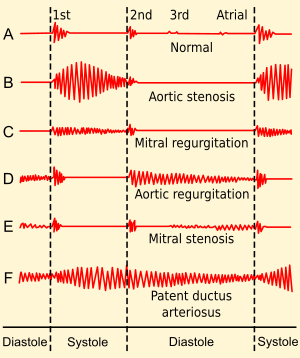
Aortic Stenosis - auscultate the carotid arteries using the diaphragm of the stethoscope whilst the patient holds their breath to listen for radiation of an ejection systolic murmur
![[z_attachments/Aortic Stenosis normal speed.mp3|Aortic Stenosis normal speed]]
-
Aortic regurgitation - sit the patient forwards and auscultate over the aortic area with the diaphragm of the stethoscope during expiration to listen for an early diastolic murmur
![[z_attachments/Aortic regurgitation normal speed.mp3|Aortic regurgitation normal speed]]
-
Mitral regurgitation - roll the patient onto their left side and listen over the mitral area with the diaphragm of the stethoscope during expiration for a pansystolic murmur. Continue to auscultate into the axilla to identify radiation of this murmur.
-
Mitral stenosis - with the patient on their left side, listen over the mitral area using the bell of the stethoscope during expiration for a mid-diastolic murmur.
Final Steps
Posterior Chest Wall
- Inspect the posterior chest wall for any deformities or scars
Auscultation
Auscultate the lung fields posteriorly:
- Coarse crackles → pulmonary oedema
- Absent air entry and stony dullness on percussion → Pleural Effusion
Sacral Oedema
Inspect and palpate the sacrum for evidence of pitting oedema.
Legs
- Inspect and palpate the patient’s ankles for evidence of pitting pedal oedema and temperature (associated with right ventricular failure).
- Inspect the patient’s legs for evidence of saphenous vein harvesting (performed as part of a coronary artery bypass graft).
To Complete the Exam
- Explain to the patient that the examination is now finished.
- Thank the patient for their time.
- Dispose of PPE appropriately and wash your hands.
- Summarise your findings.
Example summary
“Today I examined Mrs Smith, a 64-year-old female. On general inspection, the patient appeared comfortable at rest and there were no objects or medical equipment around the bed of relevance.”
“The hands had no peripheral stigmata of cardiovascular disease and were symmetrically warm, with a normal capillary refill time.”
“The pulse was regular and there was no radio-radial delay. On auscultation of the carotid arteries, there was no evidence of carotid bruits and on palpation, the carotid pulse had normal volume and character.”
“On inspection of the face, there were no stigmata of cardiovascular disease noted in the eyes or mouth and dentition was normal.” “Assessment of the JVP did not reveal any abnormalities and the hepatojugular reflux test was negative.”
“Closer inspection of the chest did not reveal any scars or chest wall abnormalities. The apex beat was palpable in the 5th intercostal space, in the mid-clavicular line. No heaves or thrills were noted.”
“Auscultation of the precordium revealed normal heart sounds, with no added sounds.” >“There was no evidence of peripheral oedema and lung fields were clear on auscultation.”
“In summary, these findings are consistent with a normal cardiovascular examination.” >“For completeness, I would like to perform the following further assessments and investigations.”
Further Assessments and Investigations
- Measure BP - lying and standing
- Peripheral vascular examination
- 12 lead ECG - look for evidence of Arrhythmias
- Dipstick urine - proteinuria or haematuria associated with Essential hypertension
- Capillary blood glucose - checking for DM
- Fundoscopy - concerns about malignant Essential hypertension