A rapid irregular atrial rhythm at 300-600 bpm. The AV node blocks most of these impulses and only responds intermittently (hence irregular QRS). Cardiac output is reduced by 10-20% as ventricles are not primed properly by atria
Main risk is from clots forming from pooling blood in atria leading to ischaemic Stroke
Causes/Factors
SMITH pneumonic:
- Sepsis - pneumonia
- Mitral valve pathology
- Ischaemia - Coronary Artery Disease
- Thyrotoxicosis
- Hypertension
Lifestyle:
- Alcohol
- Caffeine
Symptoms
- Chest pain
- Palpitations
- Dyspnoea
- Syncope/pre-syncope
- May be asymptomatic
Signs
- Irregularly irregular pulse
- 1st heart sound is of variable intensity
- Signs of underlying cause
Diagnostic Tests
- ECG

- Blood: Thyroid function test
- Echo: look at valvular (mitral/aortic) and LV function
| Paroxysmal | Persistent | Permanent |
|---|---|---|
| Episodes lasting >30 seconds but <7 days (often less than 48 hours) | Episodes lasting >7 days | Longstanding >1 year |
| Self-terminating | Not self-terminating | |
| Recurrent |
Management
Adverse features
Atrial fibrillation in patients with the follow should be defibrillated using synchronised DC cardioversion:
- Heart failure
- Myocardial ischaemia
- Shock
- Syncope
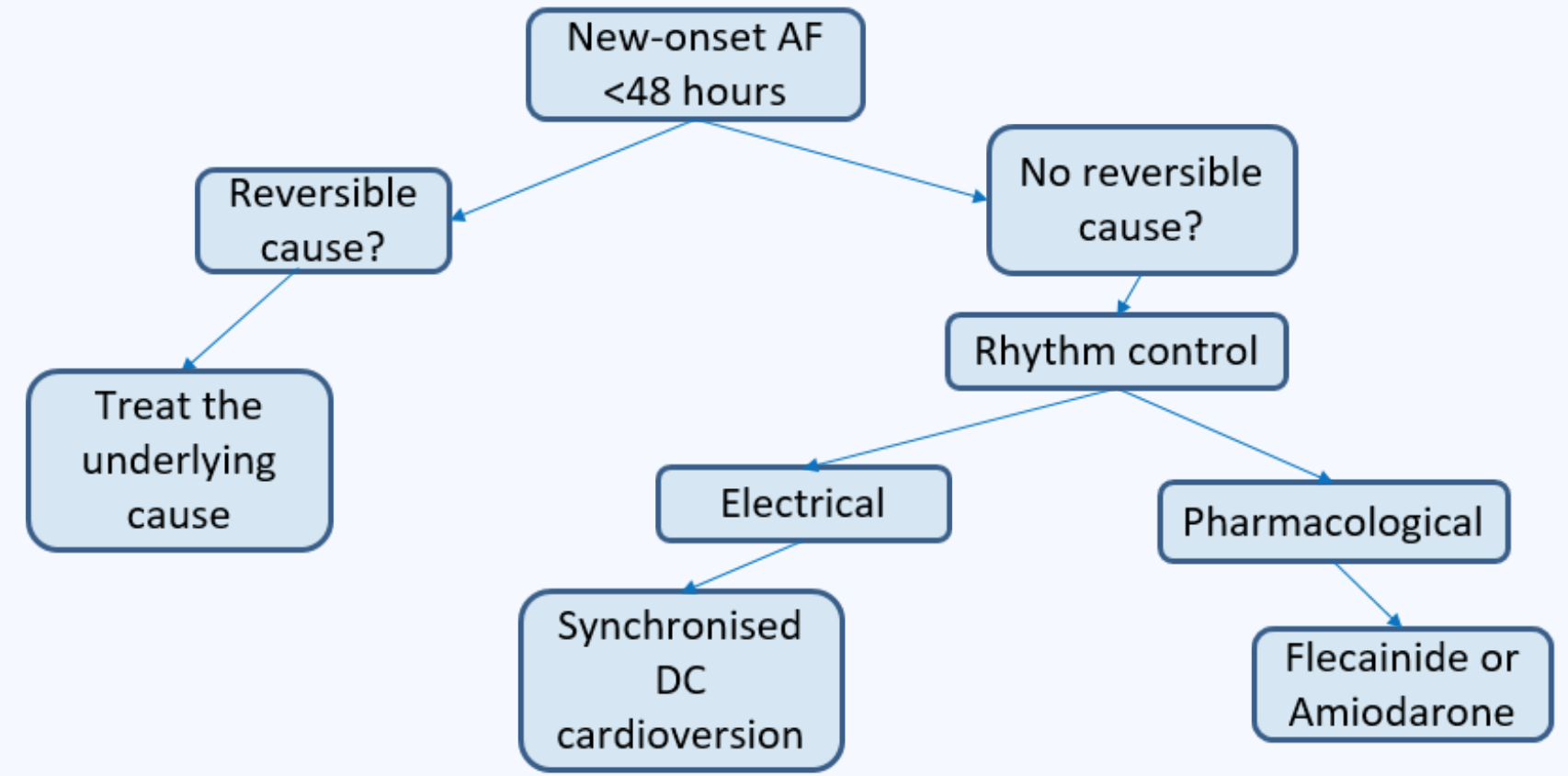
Paroxysmal AF
For intermittent short duration AF, “pill-in-the-pocket” strategy can be used. Patient can take a pharmacological cardioversion only when they feel symptoms of AF begin.
Rate control - slows down the heart rate to prevent symptom of palpitations and improve heart beat efficiency
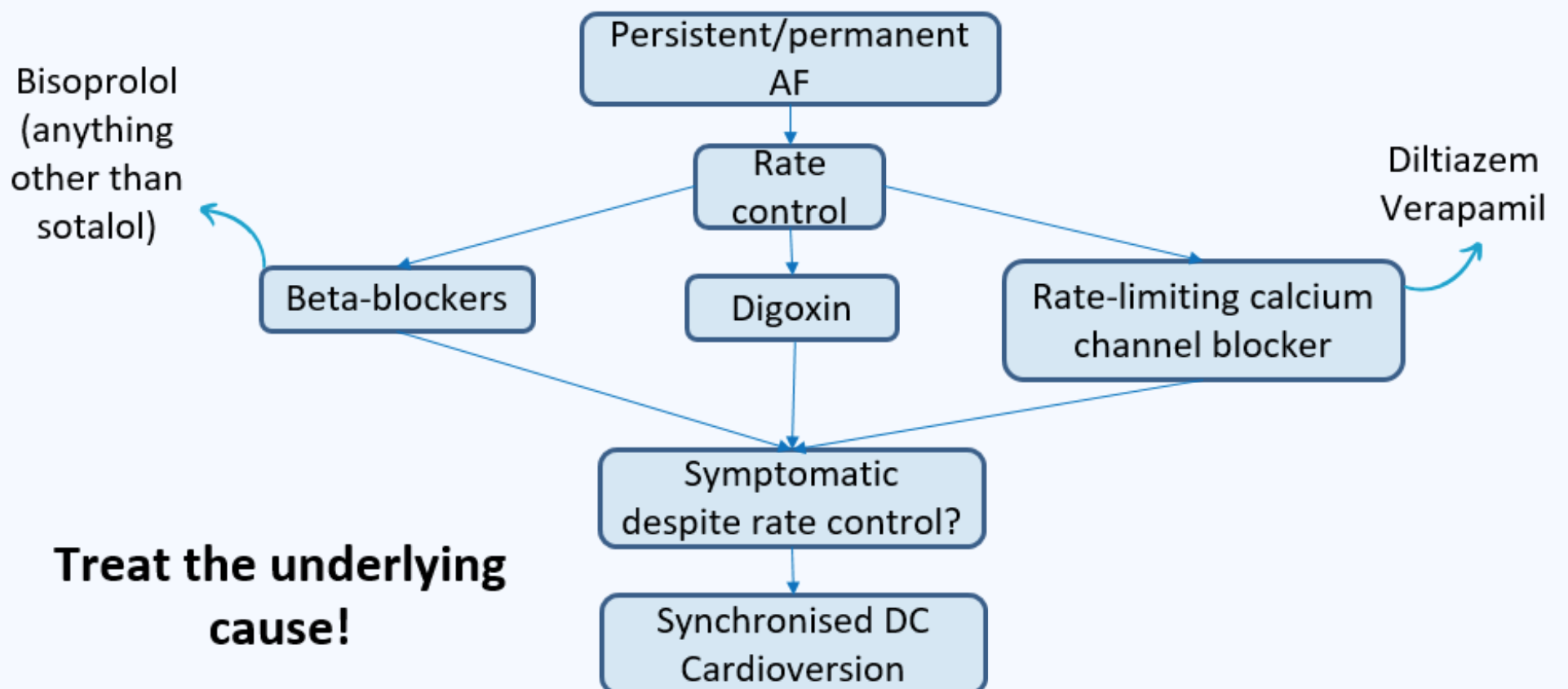
- blocker
- Calcium channel blockers (diltiazem, verapamil)
- Digoxin
Rhythm control - convert the hearth rhythm back into sinus rhythm
- Amiodarone
- Electric (DC) cardioversion
Info
Most common combination of drugs in AF is bisoprolol + apixaban
No real difference in prognosis between rate or rhythm control but rate is more common as better symptomatic improvement
Anticoagulation - CHADS-VASc score to determine whether to anticoagulate in AF. Do not withhold anticoagulation just on the basis of falls risk.
Congestive cardiac failure (1 point) Hypertension (1) Age 65-74 (1) Age 74+ (2) Diabetes (1) Stroke/TIA/thromboembolism (2) Vascular disease (1) Sex Category (1 if female)
A score of 2 = annual stroke risk of ~2-4% 3 = 3-6% risk
Increased chance of bleeding but bleeding is a better outcome than a stroke
ORBIT score used to predict risk of bleeding in AF
| Variable | Points |
|---|---|
| Haemoglobin <130 g/L (M) <120g/L for females | 2 |
| Age >74 years | 1 |
| Bleeding history | 2 |
| Renal impairment (eGFR <60) | 1 |
| Treatment with antiplatelet agents | 1 |
| No formal rules on how to act on the ORBIT score but should be taken into account. |
| ORBIT score | Risk group | Bleeds per 100 patient-years |
|---|---|---|
| 0-2 | Low | 2.4 |
| 3 | Medium | 4.7 |
| 4-7 | High | 8.1 |