95% of all hypertension without a clear underlying medical cause. It is the most important risk factor for pre-mature death and CVD.
To define hypertension the value is set at where anything above that would significantly increase risk and the benefit of treatment would be clear. Multiple measurements are needed to diagnose.
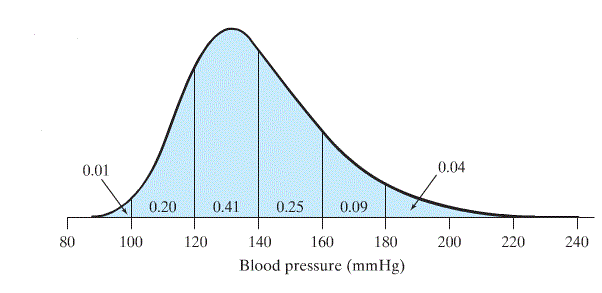
General people with consistent BP of >140/90 are considered to have hypertension.
Patient may have “White coat hypertension” - being at the doctors is an inherently nervous experience so BP. In this case may ask a patient to record their blood pressure at home
Malignant hypertension is a rapid rise in BP leading to vascular damage (fibrinoid necrosis). Usually there is severe hypertension (>200/130) + bilateral retinal haemorrhages papilledema. May be headache and visual disturbances. May cause Acute Kidney Injury, Heart Failure or encephalopathy
Secondary hypertension can be due to ROPED:
- Renal diseases which causes an imbalance in RAAS hormones.
- Obesity
- Pregnancy
- Endocrine diseases: Cushing’s Syndrome, Conn’s syndrome, etc
- Drugs
Causes/Factors
- Genetics: Family history of hypertension can increase the risk.
- Lifestyle Factors: Unhealthy lifestyle choices, including a high-salt diet, Obesity, lack of physical activity, and excessive alcohol consumption.
- Age: The risk of hypertension increases with age.
- Race: Some racial and ethnic groups are more prone to hypertension.
- Stress: Chronic stress can lead to elevated blood pressure.
Symptoms
- Usually completely asymptomatic and relies on good monitoring of patients to catch early
Diagnostic Tests
- ABPM
- 24h BP monitoring
- Fasting glucose and cholesterol to check for CVD risk factors
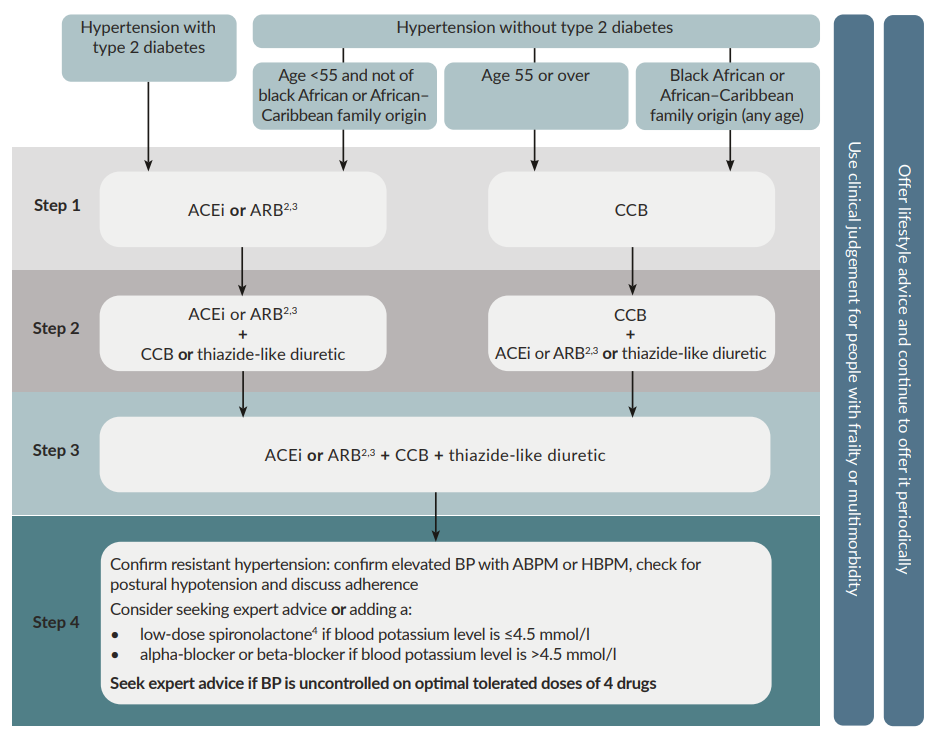
Management
Treat all >160/100. For those at 140/90 treatment depends on other comorbidities and risks but is usually done so.
Treatment goals
- <140/90 in general population
- <150/90 if ages over 80
- Life style changes - Stop smoking, low-fat diet, reduce alcohol and salt intake, increase exercise and try to lose weight
Complications/red Flags
Malignant hypertension - oral therapy unless encephalopathy or cardiac failure. Aim for controlled BP reduction over days not hours. Avoid sudden drops in BP as cerebral autoregulation is poor. Bed rest + Atenolol or long-acting CCBs
If encephalopathy monitor with arterial probe and look at guidance for IV medications needed.