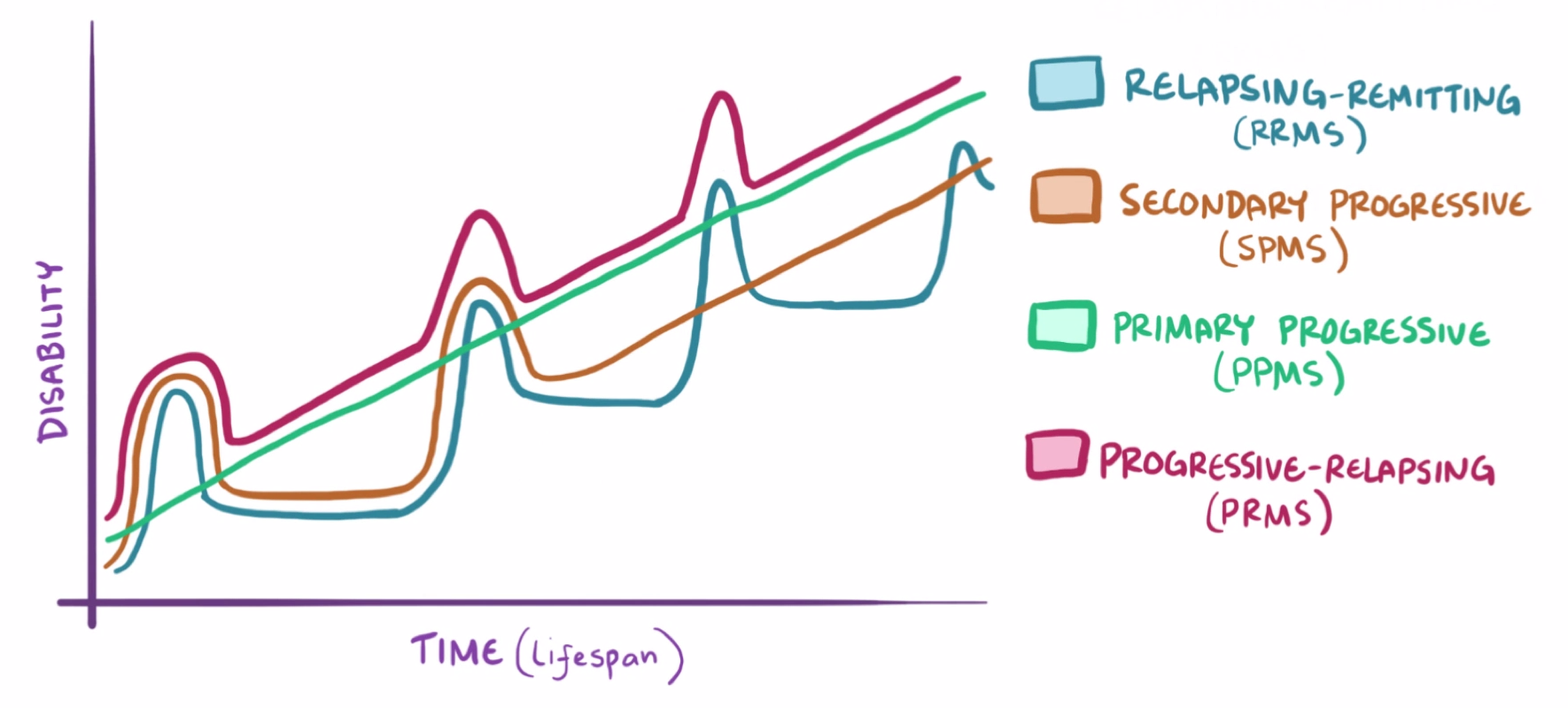
Chronic progressive autoimmune demyelinating CNS condition
- Only attacks the oligodendrocytes in the CNS
- Symptoms per episode progress over >24 hours and last days to weeks.
- Lesions vary in location so symptoms change over time - disseminated in time and space
Causes/Factors
- Age - 40-50 y/o
- Genetic susceptibility - HLA-DRB1 + many more
- EBV infection
- Smoking
- Obesity
Symptoms
Eye issues
Optic neuritis
- Central sctoma
- Pain with eye movement
- Impaired colour vision
- RAPD
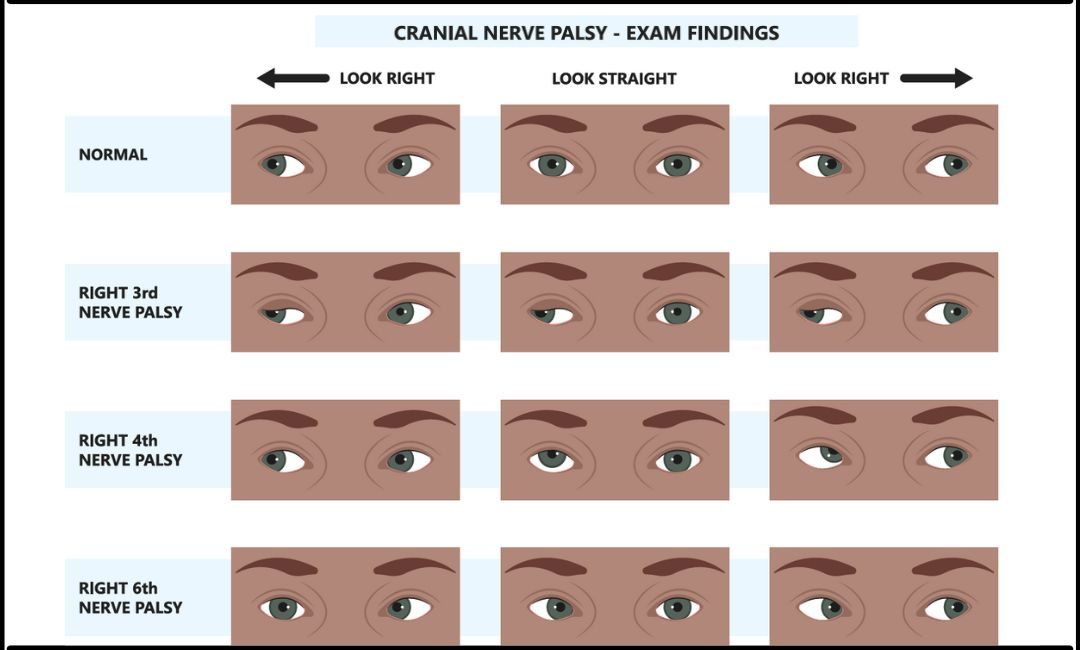
Eye movement abnormalities
Lesions can affect any cranial nerves, so Cranial Nerve Exam is important.
Focal Neurology
Breaks down into focal weakness and sensory symptoms:
-
Incontinence
-
Facial nerve palsy
-
Limb paralysis
-
Trigeminal neuralgia
-
Numbness
-
Paraesthesia
-
Lhermitte’s sign - electric shock sensation down the spine and into the limbs when flexing the neck
-
Ataxia (cerebellar lesion)
Investigations
Based on the clinical picture and symptoms suggesting lesions are changing over time. Investigations can support the diagnosis:
- MRI - typical lesions & location based on symptoms
- LP - oligoclonal bands in CSF
Management
MDT - neurologists, specialist nurse, physios & OTs
Disease-modifying therapies - big long fancy names of immunotherapy drugs
Relapses may be treated with steroids
- 500mg orally for 5 days
- 1g IV daily for 3-5 days where oral treatments fail or relapses are severe