Quick reference
Neuro exams always try to localise where in the pathway the lesion is: upper (brain, spinal cord) or lower (nerve root, peripheral nerve, NMJ or muscle). Here’s a summary of the features from UMN, remember upper, hyper
| Test | UMN signs | LMN |
|---|---|---|
| Inspection | No fasciculation or significant wasting (there may however be some disuse atrophy or contractures) | Wasting and fasciculation of muscles |
| Tone | Increased (spasticity or rigidity) +/- ankle clonus | Decreased (hypotonia) or normal |
| Power | Classically a “pyramidal” pattern of weakness (extensors weaker than flexors in arms, and vice versa in legs) | Different patterns depending on cause |
| Reflexes | Brisk (hyperreflexia) | Reduced/absent (hypo- or areflexia) |
Tests to only do for upper limb will appear blue, lower limb will be green
Gather equipment
- Tendon hammer
- Neurotip
- Cotton wool
- Tuning fork 128Hz
Introduction
- Wash hands (and don PPE if needed)
- Introduce yourself (name and role)
- Confirm patient’s name and DOB
- Explain what the examination involves
- Gain consent to continue
- Ask if patient in any pain before continuing
General Inspection
Clinical Signs
Watch gait as they walk in/ask them to walk
- Stance - ataxic gait → midline cerebellar pathology: MS, chronic alcohol exces
- Stability - staggering, slow, unsteady. Patients will lean towards the side of the cerebellar lesion
- Arm swing - often absent or reduced in Parkinson’s disease
- Steps - small, shuffling steps → Parkinsonian gait
- Turning - patients with cerebellar disease will find this difficult
Scars - previous surgery
Wasting of muscles - LMN lesion or disuse atrophy
Involuntary movements - pseudoathetosis (proprioception failure), chorea (Huntington’s)
Fasciculartions - LMN pathology
Tremor - resting, intention… etc
Romberg’s test
Possibly do but a positive test does NOT indicated cerebellar pathology - just that there is a sensory ataxia.
- Position yourself within arms reach of the patient to allow intervention to correct falling
- Ask the patient to put their feet together and keep their arms by their sides (may struggle to do this)
- Ask patient to close their eyes
Objects and Equipment
- Walking aids
- Prescription
Pronator drift
- Ask patient to close eyes
- Ask patient to hold arms out with palms facing down and then ask them to turn them over
- Observe signs of drift for 20-30 seconds
If pronator drift occurs it indicates contralateral pyramidal tract lesion
Tone
Assess tone in the muscles comparing each side
- Support patients limb
- Ask them to relax and allow you to fully control their arm
- Move all the muscle groups in all directions
- Feel for abnormalities of tone
Spasticity is associated with pyramidal tract lesions (Stroke) and rigidity extrapyramidal lesions
Velocity in tone
Spasticity is velocity dependent - the fast the movement the worse it is
Rigidity is velocity independent - it feels the same no matter the speed that you move the limb
The two main type of rigidity are:
- Cogwheel rigidity - intermittent increase in tone during movement of the limb. Due to a tremor + hypertonia. Associated with Parkinson’s disease
- Lead pipe rigidity - uniformly increased tone throughout the movement of the muscle. Associated with neuroleptic malignant syndrome
Ankle clonus
Involuntary rhythmic muscular contractions associated with UMN lesions of descending pathways (Stroke, MS, cerebral palsy). Up to 5 “beats” could be considered normal.
- Position the patient’s leg so that the knee and ankle are slightly flexed, supporting the leg with your hand under their knee
- Rapidly dorsiflex and partially evert the foot to stretch the gastrocnemius muscle
- Keep the foot in this position and observe for clonus
Power
- Assess the power by stabilising and isolating the relevant joint for each assessment. Find the list here for each movement
- You must compare both sides at the same time.
- As the patient to resist the force that you apply to the joint. Always ensure that the force you apply is proportional to the joint - eg to test finger extension use your fingers to resist.
- Communicate clear instructions for each stage of the assessment.
- Use the MRC power assessment (below) for scoring strength
| Score | Description |
|---|---|
| 0 | No contraction |
| 1 | Flicker or trace of contraction |
| 2 | Active movement with gravity eliminated |
| 3 | Active movement against gravity |
| 4 | Active movement against gravity and resistance |
| 5 | Normal power |
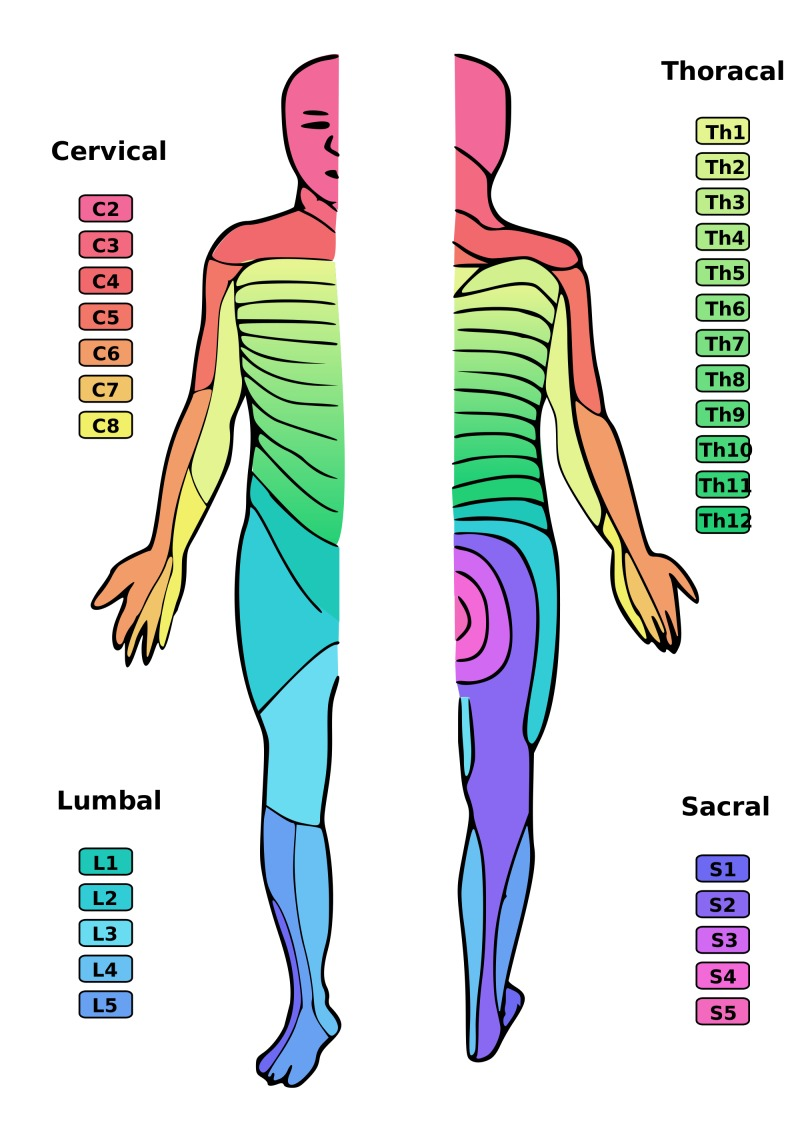
It’s important to know the Myotomes and Dermatomes and the spinal level associated with each movement.
Might be useful to know...
UMN lesions causes weaker upper limb extensions than the flexors LMN lesions cause a focal pattern - only the muscles directly innervated by the damaged nerve affected
Reflexes
For each reflex the patient’s limb needs to be completely relaxed. A trick to ensure this can be to ask the patient to clench their teeth whilst you tap the tendon to distract their mind from the limb
Biceps reflex (C5/6)
- Locate the biceps brachii tendon (antecubital fossa)
- Place thumb on over the tendon and then tap your thumb with the tendon hammer
- Observe/feel for contraction
Supinator (brachioradialis) reflex (C5/6)
- Locate brachioradialis tendon on the posterolateral aspect of the wrist approx. 4 inches proximal to base of thumb
- With 2 fingers positioned over the tendon tap fingers with tendon hammer
Triceps reflex (C7)
- Position the patient’s arm so that the triceps tendon is relaxed (rest elbow 90 flexion on their lap and/or support forearm)
- Locate triceps tendon superior to olecranon of ulna
- Tap the tendon with the tendon hammer
Knee-jerk reflex (L3/4)
- Ask patient to hang leg over side of bed. Ensure limb is completely relaxed
- Tap patellar tendon with tendon hammer
Ankle-jerk reflex (S1)
- While on bed ask support leg so hip is slightly abducted and externally rotated. The knee should be flexed and ankle in slight dorsiflexion
- Tap Achilles tendon with tendon hammer
Plantar reflex (L5-S1)
- Explain that you are going to scratch the foot with a blunt stick and it might feel uncomfortable but not painful. Gain consent
- Fix foot in position by holding ankle
- Run the blunt object along the lateral edge of the sole of the foot moving towards the base of little toe and then turn medially to run transverse across
- Observe big toe
- Normal result: flexion of the toes. Abnormal (Babinski sign): extension of big toe and abduction of other toes - suggestive of UMN lesion
Sensation
- Ensure the patient has their eyes closed for the assessment.
- Demonstrate normal sensation of the sternum each time.
- Compare left to right
- Ask the patient to say yes when they feel the sensation
Light touch
Involves both the dorsal columns and spinothalamic tracts
- Use a wisp of cotton wool to assess sensation across the upper or lower limb dermatomes.
Pin-prick
Involves the spinothalamic tracts
- Repeat over same dermatomes but with sharp end of neuro-tip
- If loss of sensation is noted distally, test for “glove distribution” associated with peripheral neuropathy
Vibration
- Tap a 128Hz tuning fork (not on a table or surface) and place on patients sternum to check they can feel it
- Tap the fork again and place onto the interphalangeal joint. Check they can correctly identify when its vibrating and when its not
- If sensation impaired continue to place the fork more proximally on more bony prominences until the patient is able to accurately identify
Proprioception
Use a distal joint e.g. thumb or big two and hold at the edges to move to prevent pressure allowing the patient to tell
- Demonstrate up and down position whilst patients eyes are open
- Ask the patient to close their eyes and ask to say what position the joint is in
- Move the joint 3/4 times in a random sequence
- If unable to identify move to more proximal joints e.g. wrist, elbow, shoulder
Coordination
Finger to nose test
- Position your finger so that the patient has to fully outstretch their arm to reach it
- Ask the patient to touch their nose with their finger and then your fingertip
- Repeat this as fast as possible
Difficulty could be due to cerebellar pathology.
Dysmetria - lack of coordination and patient may under/overshoot
Intention tremor - broad, coarse, low frequency tremor that develops as limb extends.
Careful!
Be careful not to mistake this for action tremor which is present throughout the movement
Dysdiadochokinesia
Inability to perform rapid alternating movements - feature of ipsilateral cerebellar pathology
- Ask the patient the rapidly flip one hand over in the palm of the other
- Observe the speed and fluency by which the patient can do this
- Repeat with other hand
Heel-to-shin test
Weakness from an UMN lesion can also produce apparent loss of coordination
- Ask the patient to place their left heel on their right knee and run it down their shin in a straight line
- Then ask them to return it to the starting position and repeat this movement
- Repeat this with the other leg.
To Complete the Exam
- Explain to the patient that the examination is now finished.
- Thank the patient for their time.
- Dispose of PPE appropriately and wash your hands.
- Summarise your findings.
Patterns of sensory loss
Mononeuropathies result in a localised sensory disturbance in the area supplied by the damaged nerve.
peripheral neuropathy typically causes symmetrical sensory deficits in a ‘glove and stocking’ distribution in the peripheral limbs. The most common causes of peripheral neuropathy are Diabetes Mellitus and chronic alcohol excess (B12 deficiency).
Radiculopathy occurs due to nerve root damage (e.g. compression by a herniated intervertebral disc), resulting in sensory disturbances in the associated dermatomes.
Spinal cord damage results in sensory loss both at and below the level of involvement in a dermatomal pattern due to its impact on the sensory tracts running through the cord.
Thalamic lesions (e.g. Stroke) result in contralateral sensory loss.
Myopathies often involve symmetrical proximal muscle weakness.