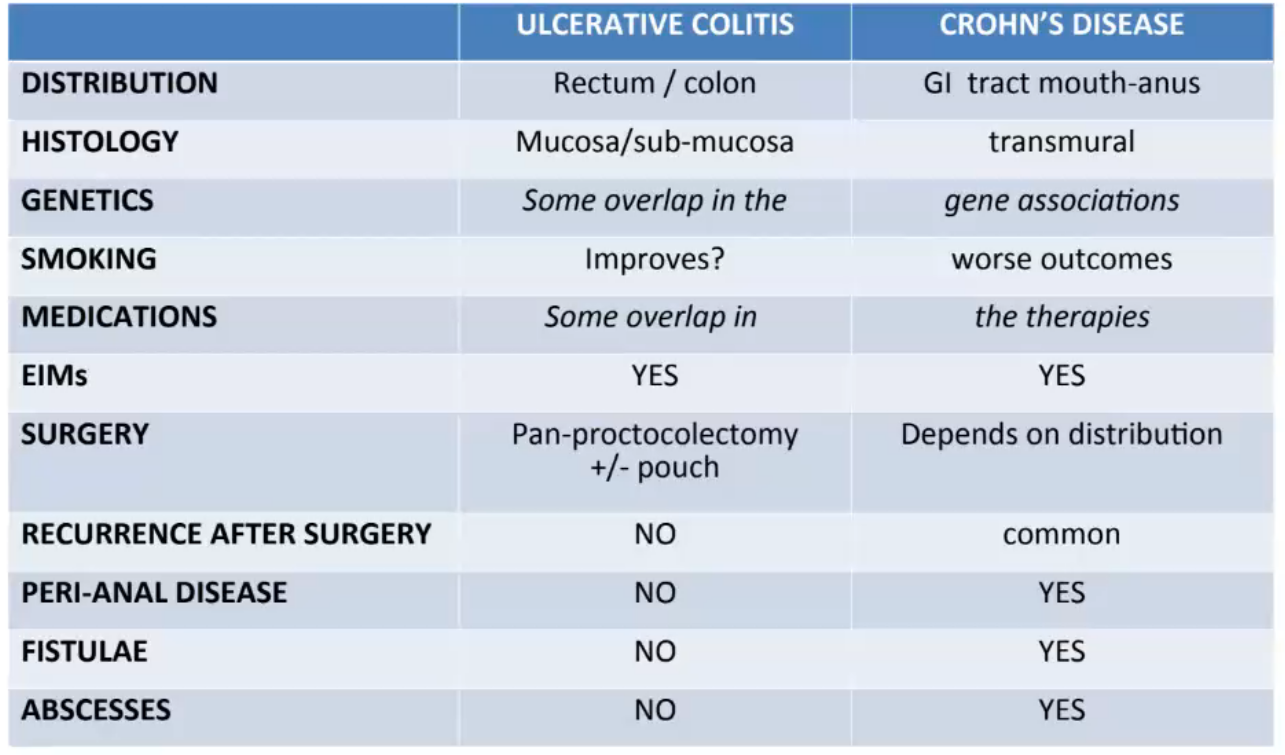
The inflammatory bowel diseases (IBD), ulcerative colitis and Crohn’s Disease are chronic autoimmune relapsing and remitting inflammation of the intestine.
Can only effect colon - “never” past ileocaecal value
 Extra intestinal manifestations
Extra intestinal manifestations
The severity of UC is usually classified as being mild, moderate or severe:
- mild: < 4 stools/day, only a small amount of blood
- moderate: 4-6 stools/day, varying amounts of blood, no systemic upset
- severe: >6 bloody stools per day + features of systemic upset (pyrexia, tachycardia, Anaemia, raised inflammatory markers)
Causes/Factors
Inappropriate immune response against (?abnormal) colonic flora in genetically susceptible individuals - failure to maintain tolerance
Symptoms
- Episodic or chronic diarrhoea mucus/blood
- Abdominal discomfort
- Bowel frequency relates to severity
- Systemic symptoms in attacks: pyrexia, malaise, anorexia
- Smoking improves condition possibly
Signs
- May be none
- Acute severe UC fever, tachycardia, distended abdomen
- Nocturnal symptoms
Extraintestinal signs:
- clubbing
- Aphthous oral ulcers
- erythema nodosum
- pyoderma gangrenosum
- episcleritis
- large joint arthritis
- ankylosing spondylitis
- nutritional deficits
Diagnostic Tests
- Calprotectin - protein released from neutrophils into stool → inflammatory marker, highly sensitive
- Blood tests for inflammatory markers/Anaemia (FBC, ESR, CRP, U&E, LFT)
- Full colonoscopy or sigmoidoscopy → biopsy
- AXR - no feacal shadows, mucosal thickening/islands
Management
Goals are to induce and maintain disease remission
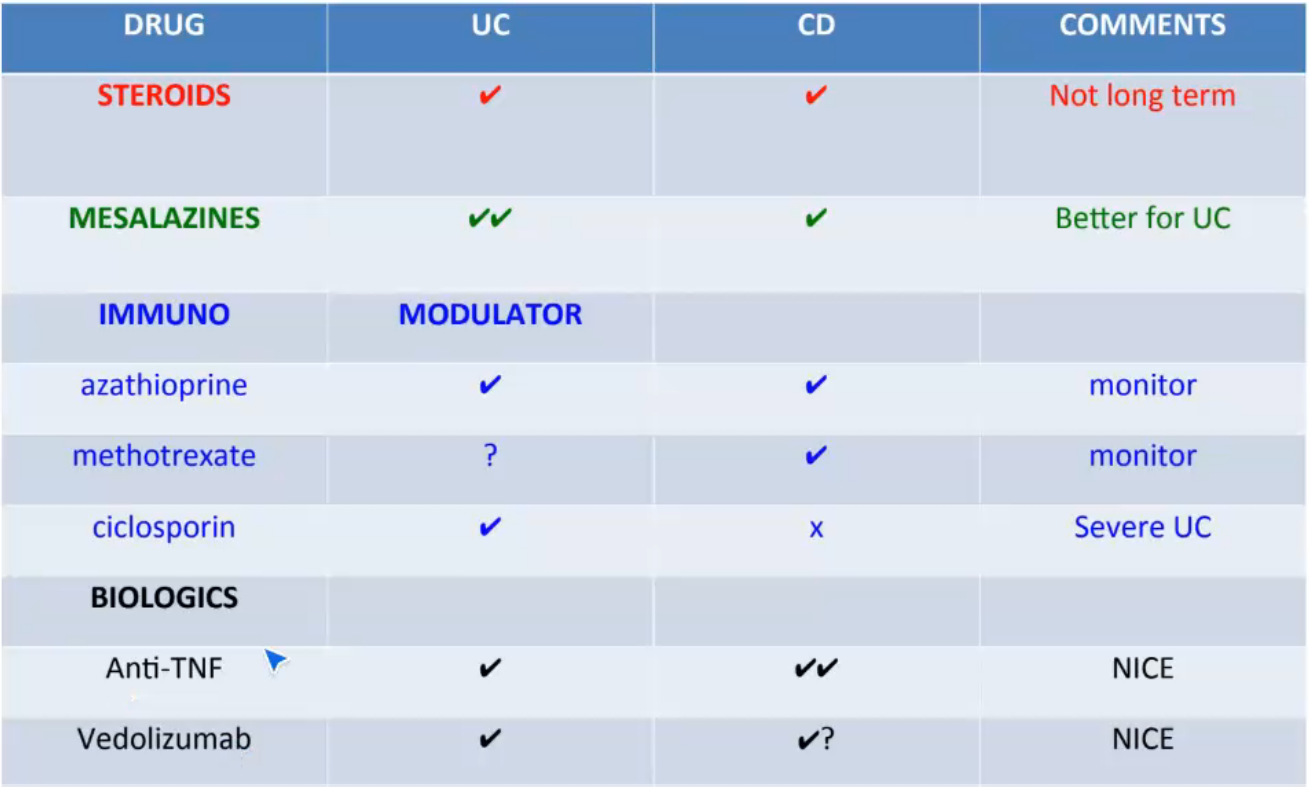
Immunomodulation if patients flare on steroid or require 2+ courses of steroid per year. Monitor LFTs. Slow acting drug compared to steroids
Biologic therapy for patients intolerant of immunomodulation or developing symptoms despite an immunomodulator
Surgery - needed at some stage in 20% of cases to remove effected part of colon
Complications/red Flags
- toxic dilation of colon (perforation risk)
- venous thromboembolism
- colon cancer