Introduction
- Wash hands (and don PPE if needed)
- Introduce yourself (name and role)
- Confirm patient’s name and DOB
- Explain what the examination involves
- Gain consent to continue
- Ask if patient in any pain before continuing
General Inspection
Clinical Signs
- Build
- Shortness of breath
- Hydration status - obvious oedema/dry skin
- Stoma bags
- Uraemic complexion - yellow colour to the skin caused by uraemia in Chronic Kidney Disease
- Cachexia - end stage renal failure
- Cushingoid appearance - high dose steroids for renal transplant or immunosuppression
Objects and Equipment
- Medical equipment - catheters, IV fluids, fistulae
- Mobility aids
- Pillows - congestive heart failure patients typically suffer from orthopnoea
- Vital sign charts
- Fluid balance charts
- Prescription
Hands NOT IN EBOOK
Inspection
- Pallor - anaemia (EPO deficiency)
- Fingerprick marks secondary to capillary glucose test
- Tremor - can be caused by immunosuppressive medication
- Koilnychia/leukonychia
- Lindsay’s half-and-half nails - white discolouration of the proximal portion of the nail and red/brown colour of distal portion
Asterixis (flapping tremor)
In context of urological exam most likely underlying cause is hepatic encephalopathy (due to hyperammonaemia) or uraemia secondary to renal failure. retention is another possible cause.
- Ask patient to stick arms out and cock hands back for 30 seconds
Skin turgor
Well-hydrated skin should spring back to previous position immediately whereas dehydrated ski will slowly return to normal
- Assess by gently pinching a fold of skin on the back of the hand and releasing after a few seconds
Arms
Inspect
Inspect the arms for signs of:
- Excoriation - pruritis secondary to uraemia
- Brusing - excessive steroid use or platelet dysfunction
- Skin lesions - Warts of skin cancers associated with immunosuppression
- AV fistula - wrist, ACF common sites. Palpate for thrill and auscultate if present
Palpate
Radial pulse
- Character, rate and rhythm
Blood pressure
Tell the examiner that you would like to take one
Causes include Chronic Kidney Disease, renal ransplant rejection, cortiosteroid use, tacrolimus or ciclosporin. Rarely pulsus paradoxus (change of >10mmHg during breathing)
Danger
Blood pressure should not be performed on the side of an AV fistula!!
Respiratory rate
Also offer to do and explain how you would do it Whilst still palpating the radial pulse assess the patient’s respiratory rate. Note any asymmetries in expiratory and inspiratory phases
- Report breathing pattern and respiratory effort. Asymmetries in breathing , tachypnoea, bradypnoea
Face NOT IN EBOOK
General
- Skin colour and lesions - uraemic frost, Squamous cell carcinoma, Basal Cell Carcinoma
- Cushingoid appearance
- Hypertrichosis - excessive hair growth. A side effect of ciclosporin
- Hearing aid - consider Alport syndrome
Eyes
- Conjunctival pallor - anaemia
- Band keratopathy - deposition of calcium to the central cornea. Chronic hypercalcaemia
- Periorbital oedema - clinical feature of Nephrotic syndrome
Neck
Inspection
- Dialysis catheter at base of neck
- Small scar at the base of the neck suggesting a parathyroidectomy
Jugular Venous Pressure
- Position the patient in a semi-recumbent position (at 45°).
- Ask the patient to turn their head slightly to the left
- Inspect for evidence of IJV running between the medial end of the clavicle and the ear lobe, under the medial aspect of the sternocleidomastoid
- Measure the JVP by assessing the vertical distance between the sternal angle and the top of the pulsation point of the IJV (in healthy individuals, this should be no greater than 3 cm).
An elevated JVP indicates increased central venous pressure secondary to fluid overload. Patients in end-stage renal disease become anuric and often develop fluid overload
Abdomen
Reposition the patient to completely supine
Inspect
- Scars - previous surgeries
- Peritoneal dialysis catheter
- Abdominal distension - Polycystic Kidney Disease, Nephrotic syndrome (Ascites)
- Nephrostomy tube
- Striae
- Distension
Abdominal Palpation
Ask the patient if they are aware of any areas of abdominal pain (if present examine last). Keep good eye contact to look for discomfort.
Light Palpation of the Abdomen
- Tenderness
- Rebound tenderness: said to be present when the abdominal wall, having been compressed slowly, is released rapidly and results in sudden sharp abdominal pain. Weakly associated with peritonitis
- Voluntary guarding: contraction of the abdominal muscles in response to pain
- Involuntary guarding/rigidity: involuntary tension in the abdominal muscles that occurs on palpation associated with peritonitis (e.g. appendicitis, diverticulitis).
- Masses: large or superficial masses (e.g. hernias) may be noted on light palpation.
Deep Palpation
Warn the patient this may feel uncomfortable - carefully monitor face If any masses are identified during deep palpation, assess the following characteristics:
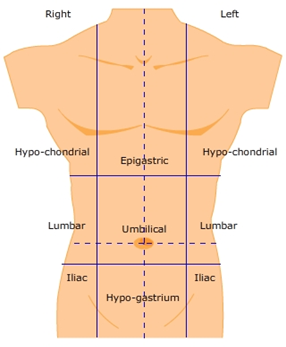
- Location: note which of the nine abdominal regions the mass located within.
- Size and shape: assess the approximate size and shape of the mass.
- Consistency: assess the consistency of the mass (e.g. smooth, soft, hard, irregular).
- Mobility: assess if the mass appears to be attached to superficial or underlying structures.
- Pulsatility: note if the mass feels pulsatile, suggestive of vascular aetiology (e.g. abdominal aortic Aneurysm).
Pay particular attention to the supra-pubic region. A distended bladder will be dull on percussion
Ballot the kidneys
-
Place hands in this position and push fingers together

-
Ask patient to take a deep breath and feel for kidney moving down
-
If kidney ballotable describe size and consistency
-
Repeat on other side In healthy individuals the kidneys are not usually ballotable but in low BMI patients might be possible
- Bilaterally enlarged - Polycystic Kidney Disease or amyloidosis, hydronephrosis
- A unilaterally enlarged - Renal Cell Carcinoma renal tumour.
How to distinguish enlarged spleens from enlarged kidneys
- Unable to get above the spleen
- A notch is palpable in an enlarged spleen
- On inspiration the kidney moves inferiorly but spleen inferiomedially
- The kidney is ballotable
Abdominal Percussion
- All 9 areas
- Towards the spleen
- Bladder
Causes of a distended bladder
Outlet obstruction:
- Faulty valves (children)
- Benign Prostatic Hyperplasia or Prostatic Adenocarcinoma
- Urethral stricture
Decreased bladder tone
- Neurogenic Bladder (spinal cord injury)
- Detrusor failure (chronic retention)
Posterior abdominal exam
Ask the patient to sit up on the edge of the bed
Palpation
- Palpate gently the renal angles
- Tenderness of the ribs or para-spinal muscles is not renal in origin
Renal angle tenderness suggests:
- Pyelonephritis
- Renal or perirenal abscess
- Acute hydronephrosis
To Complete the Exam
- Explain to the patient that the examination is now finished.
- Thank the patient for their time.
- Dispose of PPE appropriately and wash your hands.
- Summarise your findings.
Further Assessments and Investigations
- Stool sample
- Hernial examination - inguinal
- Rectal exam
- Urine analysis
- Genitalial examination