- type 1 diabetes – where the body’s immune system attacks and destroys the cells that produce insulin ^7f5ee9
- Latent autoimmune diabetes in adults
- type 2 – where the body does not produce enough insulin, or the body’s cells do not react to insulin
- Maturity onset DM of the young (MODY) - monogenic forms of diabetes that are characterized by early-onset diabetes. Autosomal dominant
| Type I | Type II | |
|---|---|---|
| Aetiology | Autoimmune (-cell destruction) | Cells become insulin resistance and -cell dysfunction |
| Presentation | Young (12 y/o peak) slim, osmotic symptoms, weight loss (days to weeks), Diabetic ketoacidosis | Older (60 y/o) osmotic symptoms, diabetic complications (months-years), usually obese |
| Treatment | Insulin (match size of meals) | Diet, exercise, oral hypoglycemics, insulin later |
- Gestational diabetes
Secondary
- Pancreatic destruction (pancreatitis, Cystic Fibrosis)
- Cushing’s Syndrome
Presenting Features
- Polyuria
- Polydipsia
- Weight loss
- Fatigue
- Pruritis vulvae and balanitis
- vaginal candidiasis
- Hunger
- Blurred vision (can be cured)
Diagnostic Tests
If symptomatic a single abnormal test is enough, if asymptomatic two abnormal tests are required
- Symptoms and random plasma glucose >11 mmol/L
- Fasting plasma glucose >7 mmol/L
- HbA1C - 48 mmol cut off for starting treatment
Weight loss, short history and moderate or large urinary ketones are indication for immediate insulin treatment at any age
Pre-diabetes is described as an HbA1c of 42-47 mmol/mol
Management
Type 1
Usually basal bolus injections (once or twice daily long acting insulin + premeal quick acting insulin). Need to judge carbohydrate intake and aware of blood glucose lowering in exercise. Possible insulin pump.
Type 2
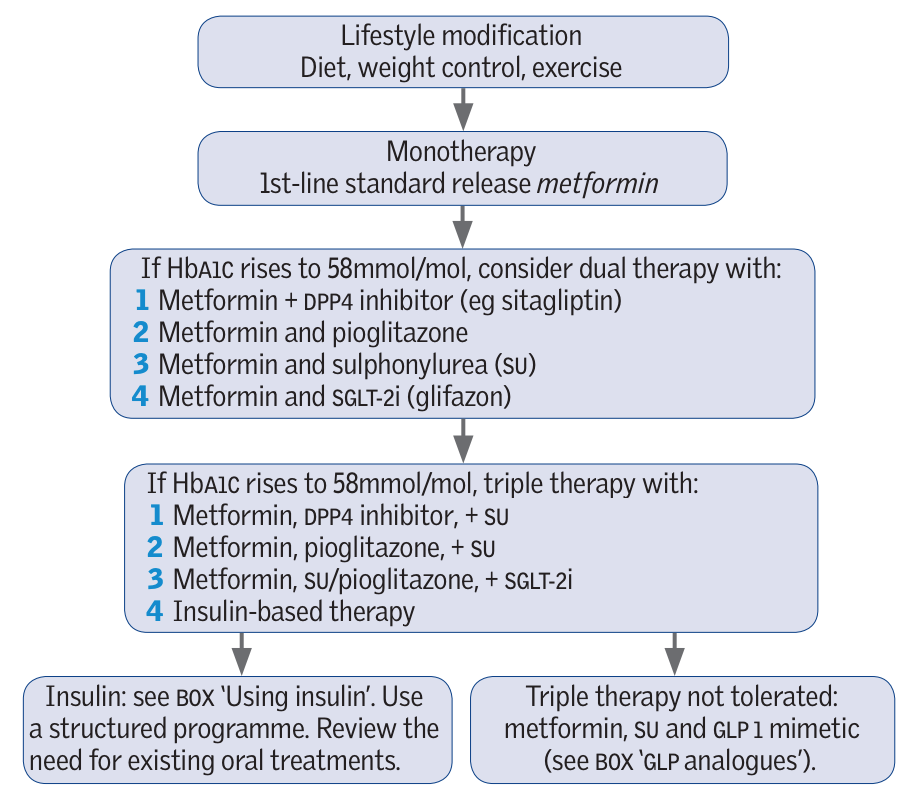
Life style modification. metformin + combination with other drug possibly
Targets:
- 48 mmol/mol for new type 2 diabetics
- 53 mmol/mol for patients requiring more than one antidiabetic medication
The HbA1c is measured every 3 to 6 months until under control and stable
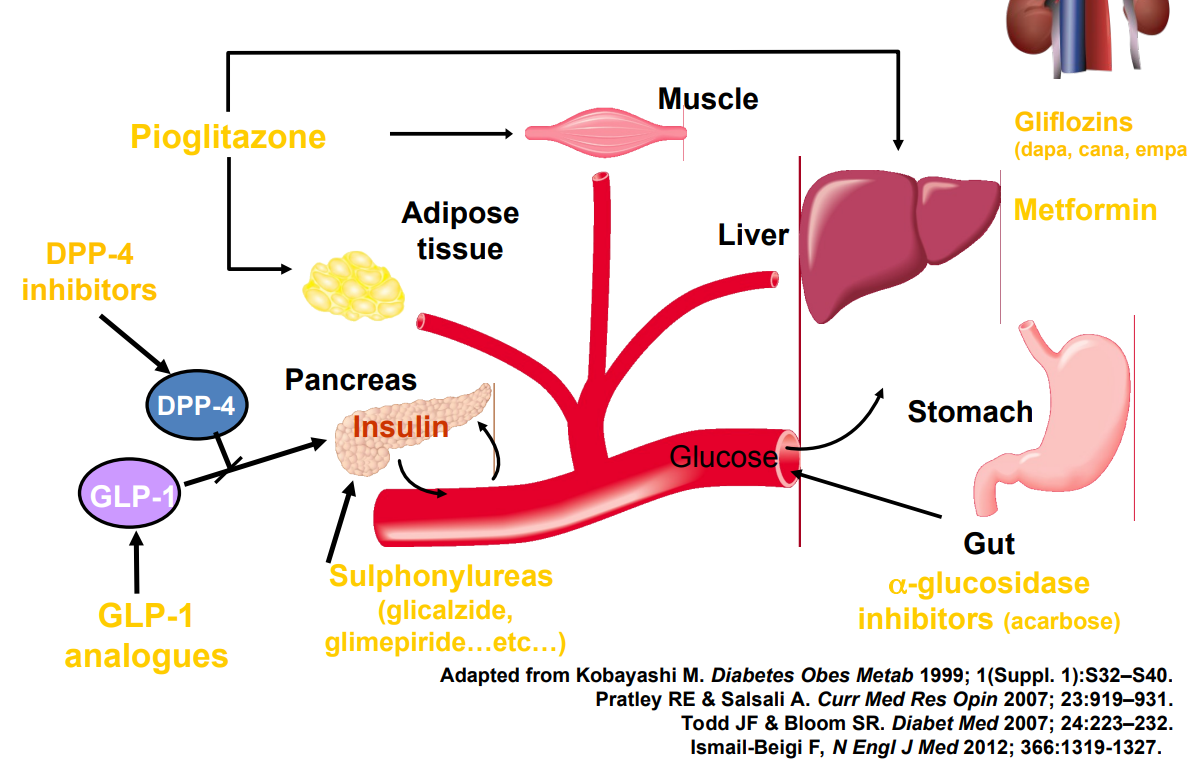
Hypoglycaemic agents:
First line
- Metformin: A biguanide - insulin sensitivity + decreases liver glucose production (may help weight).
- Avoid if eGFR is <36.
- GI symptom side effects (can switch to modified release) + risk of lactic acidosis when in AKI.
(some recommendations to consider as first line treatment)
- SGLT2i - sodium glucose co-transpoter 2 inhibitor. Blocks the reabsorption of glucose in kidneys - wee out sugar. eg Empagliflozin
- Once settled on metformin and the patients has cardiovascular risk (pre-existing or Q-risk score >10%) add SGLT2i.
- Can increase risk of hypoglycaemia
- Reduces cardiovascular risk, lowers HbA1c, lowers BP improves features of heart failure
- Increases frequency of urinary tract infections and genital thrush and rarely risk of DKA (even with a moderately increased glucose). Rare risk of necrotising fasciitis of the genitalia or perineums
Second line
- DPP4 inhibitors/gliptins - block enzyme which destroys the hormone incretin (stimulates a decrease in blood glucose levels) eg sitagliptin - few side effects (headaches, rarely pancreatitis)
- Glitazone - insulin sensitivity, LFTs needed every 8 weeks - do not use in patient with Heart Failure eg pioglitazone
- Decreases the liver production of glucose
- Side effects of: weight gain, heart failure, bone fractures, bladder cancers
- Sulfonyurea - insulin secretion but increased cardiovascular morbidity and mortality - promote weight gain eg Gliclazide
- GLP-1 Mimetics: incretin analogues - suppress appetite. Weight loss effect
Insulin
Insulin is usually initiated and managed by diabetic specialist nurses
| Insulin | Time | Example |
|---|---|---|
| Rapid acting insulins | Acts in 10 mins lasts for 4 hours | NovoRapid |
| Short acting insulins | Acts in 30 mins lasts for 8 hours | Actrapid |
| Intermediate-acting insulins | Acts in 1 hours and lasts for 16 hours | Humulin I |
| Long-acting insulins | Acts in 1 hours and lasts for 24 hours | Levemir |
Combinations insulins contain a rapid-acting and intermediate-acting Insulin. In brackets is the ratio of rapid-acting to intermediate-acting Insulin:
- Humalog 25 (25:75)
- Humalog 50 (50:50)
- Novomix 30 (30:70)
Tip
A common exam scenario involves discussing the possibility of starting Insulin with an HGV driver. Patients treated with Insulin must fulfil very strict criteria to carry on driving, so starting Insulin has enormous implications for professional drivers. This can be a motivating factor for improving diet, exercise and taking medications to improve diabetes control and avoid Insulin.
Complications/red Flags
Hypoglycaemia - due to too high Insulin → coma and brain damage, thrombosis, cardiac Arrhythmias
Infections - periodontitis, thrush and infected ulcers
Type 1 diabetes
- if a patient is on Insulin, they must not stop it due to the risk of Diabetic Ketoacidosis
- check blood glucose more frequently, for example, every 1-2 hours including through the night
- consider checking blood or urine ketone levels regularly
- maintain normal meal pattern if possible
- if appetite is reduced meals could be replaced with carbohydrate-containing drinks (such as milk, milkshakes, fruit juices, and sugary drinks)
- aim to drink at least 3 L of fluid (5 pints) a day to prevent dehydration
Type 2 diabetes
- advise the patient to temporarily stop some oral hypoglycaemics during an acute illness
- medication may be restarted once the person is feeling better and eating and drinking for 24-48 hours
- Metformin: stop treatment if there is a risk of dehydration, to reduce the risk of lactic acidosis.
- sulfonylureas: may increase the risk of Hypoglycaemia
- SGLT-2 inhibitors: check for ketones and stop treatment if acutely unwell and/or at risk of dehydration, due to the risk of euglycaemic DKA
- GLP-1 receptor agonists: stop treatment if there is a risk of dehydration, to reduce the risk of AKI
- if on Insulin therapy, do not stop treatment, as above
- monitor blood glucose more frequently as necessary
Essential hypertension and Chronic Kidney Disease - ACEi
Erectile dysfunction - sildenafil or tadalafil
Microvascular
- Diabetic eye disease - regular eye test
- Neuropathy - regular foot exam / nerve conduction. There are four options for neuropathic pain (e.g., Diabetic neuropathy):
- Amitriptyline – a tricyclic antidepressant
- Duloxetine – an SNRI antidepressant
- Gabapentin – an anticonvulsant
- Pregabalin – an anticonvulsant
- Nephropathy - urine test for albumin - Chronic Kidney Disease
Macrovascular
Hyperosmolar hyperglycaemic state
Rare but potentially fatal complication.
Hyperosmolality - water loss leading to very concentration blood Hyperglycaemia - with the absence of key tones - different from Diabetic ketoacidosis
- Presentation: polyuria + polydipsia, weight loss, dehydration, tachycardia, hypotension, confusion
- Medical emergency - escalate. Treat with IV fluids