- Chronic obstructive pulmonary disease
- A common slowly progressive disorder characterised by airway obstruction
- Little to no reversibility (how to differentiate from asthma)
- Includes chronic bronchitis and emphysema
- Patients usually have either COPD or asthma not both
Pink puffers and blue bloaters - likely ends of the spectrum:
Pink puffers - emphysema
- have alveolar ventilation near normal and a normal or low
- breathless but not cyanosed
- may progress to Type I
Blue bloaters - chronic bronchitis
- have alveolar ventilation with a low and a normal or low
- cyanosed but not breathless
- may go on to develop cor pulmonale
- respiratory centres relatively insensitive to and rely on hypoxic drive to maintain respiratory effort
Causes
Smoking, pollution
Symptoms
- Productive cough
- Dyspnoea
- Wheeze
Signs
- Tachypnoea
- Use of accessory muscles for respiration
- Hyperinflated chest
- Decreased breath sounds
Diagnostic Tests
- Spirometry: predicted, ratio <0.7
- CXR: hyperinflation, large central pulmonary arteries
- ABG: hypercapnia
Management
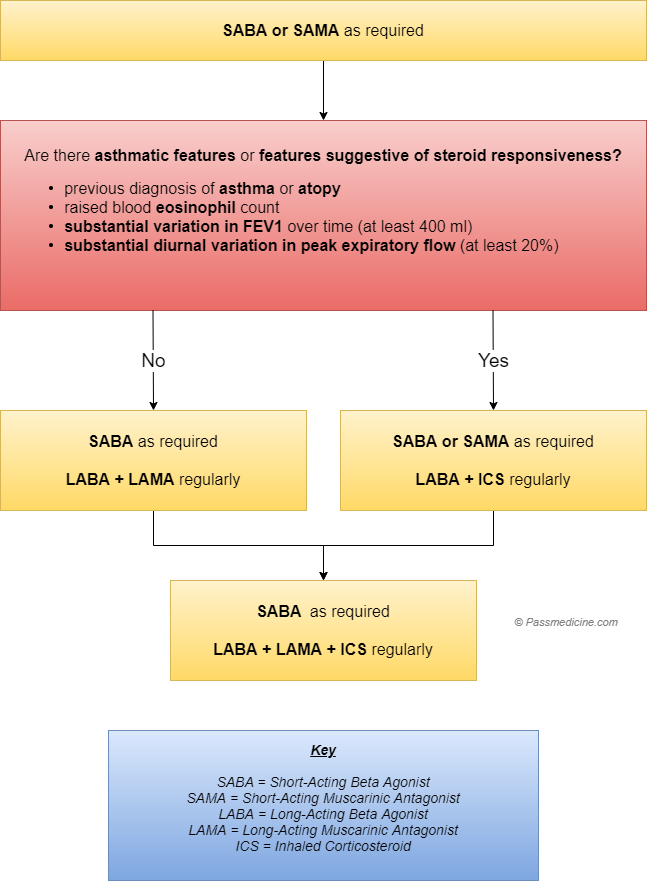
- Initial treatment: short acting agonist (SABA) (Salbutamol) and short acting muscarinic antagonist (SAMA) (Ipratropium Bromide) - as necessary
Step up if no asthma features: LABA + LAMA
Step up treatment when symptoms and exacerbations are still a problem with asthma/steroid responsive features:
- Inhaled corticosteroids
- Oral steroids (for exacerbation for 5 days)
- Mucolytics
- Long-term therapy (NICE guidelines, targets of 88-92%)
During exacerbations, to keep them out of hospital prescribe short course of steroids ± antibiotics - Azithromycin to Avoid infections (250mg TDS)
Non-invasive ventilation should be considered in all patients with an acute exacerbation of COPD in whom a respiratory acidosis
Patients should have the pneumococcal and annual flu vaccine.
Complications
- polycythaemia - increased haematocrit
- Respiratory Failure
- pneumothorax
- cor pulmonale